
March 01, 2020
Vaccine hesitancy
Dr. Sarah J. Wooten, a small animal veterinarian from Greeley, Colorado, has had first-hand experience with clients who are concerned about vaccinations but says listening to their concerns without judgment may be beneficial.
“People are afraid of what the vaccines may do to their pets,” she said. “The intentions of people that don’t want to vaccinate are pure. They just want their pets to be healthy and they’re afraid.” Dr. Wooten retired from clinical practice and is now a public speaker and author.

In recent years, human medicine has faced a growing number of individuals who reject mainstream science regarding the safety and efficacy of vaccines. In the same vein, many veterinary professionals say that, increasingly, they are hearing concerns from pet owners regarding the safety or necessity of vaccines for their pets.
Many websites that identify as natural or holistic warn about the dangers of over-vaccination of dogs and cats, but none define what they mean by over-vaccination. All agree, for most vaccines, that annual revaccination is unnecessary, but that is generally consistent with recommendations from the AVMA and other major organizations.
Some of these same sites warn about the potential long-term harms of over-vaccination, especially the potential for immune-mediated disease and cancer, but none provide any information on the specific types of diseases and cancers they associate with over-vaccination or the incidence. And none provide any data proving a cause-and-effect relationship between over-vaccination and these long-term concerns.
Still, in 2019, only 66% of dog, cat, and rabbit owners in the U.K. said their pet had its primary vaccinations when young, compared with 84% in 2016, according to the PDSA Animal Wellbeing Report, an annual analysis of overall pet well-being in the U.K.
However, despite this apparent increase in the reluctance to vaccinate their pets, most pet owners are willing to discuss the issue and just want their concerns to be heard and validated, according to veterinarians with whom JAVMA News spoke.
The trend has not gone unnoticed. The World Health Organization listed vaccine hesitancy as one of the top global threats in 2019, and the theme of the World Veterinary Association’s 2019 World Veterinary Day was the “Value of Vaccination.”
Current efforts
The World Small Animal Veterinary Association has also observed the increase in hesitancy among clients and is surveying companion animal veterinarians about the issue to better understand the phenomenon. The association defines vaccine hesitancy as a “delay in acceptance or refusal of vaccines despite availability of vaccination services.”
Dr. Michael Day, chairman of the WSAVA Vaccination Guidelines Group, said lower herd immunity is one of the biggest concerns around this issue, as it means that well-controlled infectious diseases might become problematic again.
“As I travel the world speaking to veterinarians about vaccination, it is clear that vaccine hesitancy is of great concern to our colleagues in practice,” Dr. Day said. “Interestingly, the phenomenon appears to exist in both mature and developing veterinary markets.”
Dr. Day is emeritus professor of veterinary pathology at the University of Bristol, U.K., and adjunct professor of veterinary pathology at Murdoch University in Western Australia.
“These are difficult discussions for any veterinarian to have with clients who may firmly believe that vaccines are a potential danger to their pets,” he said. “Veterinarians need to adopt a nonconfrontational but persuasive communication style to convey correct, science-based information in an understandable fashion.”
To facilitate that conversation, the AVMA has several vaccination-related resources available for pet owners. AVMA members can also download a handout version of the materials.
The WSAVA group also developed a resource document (PDF) intended for owners and breeders. The document discusses infectious disease, the immune system, vaccination, and vaccination protocols.
WSAVA created the vaccine hesitancy online survey for companion animal veterinarians to understand better why owners decline vaccination for their animals, even when vaccines are affordable and readily available. It closed at the end of January for analysis; the data will be released publicly in September.
The conversation
 Dr. Catherine M. Brown, Massachusetts state epidemiologist and public health veterinarian, has received calls about vaccine hesitancy from veterinarians as well as questions about it at veterinary conferences.
Dr. Catherine M. Brown, Massachusetts state epidemiologist and public health veterinarian, has received calls about vaccine hesitancy from veterinarians as well as questions about it at veterinary conferences.
“I think it is something that everybody is struggling with, and they want to provide good guidance for their clients. They don’t want to coerce them but they also want to make sure the animal gets everything that is appropriate,” Dr. Brown said.
She said the exposure risk for rabies, specifically, varies across the United States and depends on what variant of the virus is circulating in the area. But there is always a chance that any individual animal could come into contact with an infected wild animal.
She added that it is important to note that the U.S. has eliminated the dog variant of the rabies virus from circulation.
“It (rabies) is not in your face as much and therefore people—all of us, veterinarians and the public—sometimes forget what a significant risk rabies still can be,” Dr. Brown said. “I think we’re seeing the same thing in human medicine with measles, mumps, and rubella. … We see them a lot less frequently so people feel like, ‘Why do I have to vaccinate?’ And to be fair, I think it’s a reasonable question to ask.”
Dr. Brown said she usually speaks to people about the risk of rabies and other diseases, as well as shares data on the safety of vaccines. She noted that there are potential adverse effects for any vaccine but that the number of animals that react poorly to the vaccine is small.
Dr. Wooten agrees that sharing information while also trying to understand the client’s perspective helps. For example, a pet owner may say they don’t want autism in their dog or cat and that they’re more afraid of autism than of distemper, parvovirus, or rabies.
“I think the main thing is accepting where the pet parent is at, even if they are on a different planet than you,” Dr. Wooten said.
She suggests asking a pet owner about why they have such beliefs and where they got the information.
“It can be something like: ‘You are as much a decision-maker about your pet’s health as I am.… Tell me more about why you think that. Tell me more about where you got that information.’ And then, just shut your mouth and listen. … I find when you give people a chance to share their piece, to share their knowledge—even if it’s erroneous—they feel heard, they feel validated, they feel respected. And then, if you ask for permission to share what you know about vaccine safety, efficacy, and the diseases they protect against and you allow the pet parent to make the decision based on all of that information, then you’ve done your part.”
On the books
Legally, pet owners in some states are required to vaccinate their dogs and cats against rabies. Some states prescribe a specific interval, while others refer to the label of the vaccine used or the Compendium of Animal Rabies Prevention and Control. Some states do provide exemptions to their vaccination requirements if medically necessary as determined by a veterinarian.
The AVMA has compiled a summary of the various state laws on rabies vaccination (PDF).
Importantly, although owners may be legally required to vaccinate their animals against rabies, other vaccines may not be required by law.
The WSAVA global vaccination guidelines list core vaccines for dogs as those that protect against canine distemper virus, canine adenovirus, and the variants of canine parvovirus type 2. Core vaccines for cats include those that protect against feline parvovirus, feline calicivirus, and feline herpesvirus-1, according to the WSAVA global guidelines for the vaccination of dogs and cats, released in January 2016. The Vaccination Guidelines Group recognizes that particular countries will identify additional vaccines that they consider core.
The American Animal Hospital Association updated its canine vaccination guidelines in 2017 and 2018. The guidelines are developed by the AAHA Canine Vaccination Guidelines Task Force. The American Association of Feline Practitioners also has cat-specific vaccination guidelines.
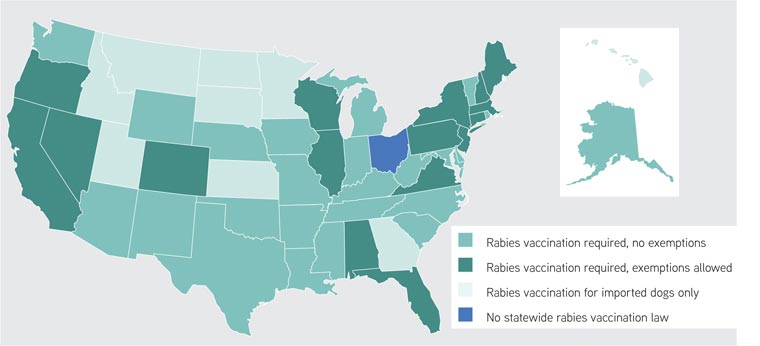
Source: Information compiled from the AVMA, state websites, and the Animal Legal and Historical Center at the Michigan State University College of Law
Continued challenges
As the industry continues to face challenges around this topic, veterinary students are learning about how to speak to clients about vaccination.
Dr. Christopher R. Lea, an assistant clinical professor at Auburn University College of Veterinary Medicine, tries to include communication skills in the curriculum, including how to discuss vaccines.
“Twenty years ago, people never asked me about that. Now, people are more educated about vaccines, and they will ask more about safety and about risk,” Dr. Lea said. “We are trying to train our veterinarians to be educated about that and be able to answer those questions.”
Dr. Lea is one of two faculty members who direct Auburn’s Veterinary Clinic, designed to provide preventive and wellness care for animals while providing fourth-year veterinary students with the educational experience of running a community practice.
He said when people come into the veterinary clinic who are hesitant to vaccinate, the students and veterinarians do their best to communicate their expertise.
“Sometimes they take our recommendations, and sometimes they don’t,” Dr. Lea said. “At the end of the day, they’ll make the decision for their cat, and you know, at that point we tell students, ‘You make your recommendation, and if they choose not to do that, you make some sort of medical record that it was discussed and declined, and then you move on.’”
Dr. Wooten believes that education and an open dialogue are key to curbing vaccine hesitancy.
“I think the main thing that we need to address is a combination of misinformation, usually from the internet, and then fear,” Dr. Wooten said. “You have to be open and curious about where that person is coming from.”
A script for discussing vaccines with a concerned client
Dr. Sarah J. Wooten, a small animal veterinarian from Greeley, Colorado, suggests the following script, first published in October 2017 in dvm360 magazine, for veterinarians discussing vaccines with a concerned client.
The veterinary professional: Bella is due for her vaccines.
Client: I don’t want to have Bella vaccinated today.
The veterinary professional: Can you tell me your main concern with vaccination?
Client: I’m just not interested.
(This is when you need to finesse this conversation a little to get the client to open up.)
The veterinary professional: No pressure at all. I really just want to know what your concerns are so we can do the best thing for your pet.
(Client may get squirmy or evasive.)
Client: Well, I read that vaccines can cause autism.
The veterinary professional: Thanks for telling me, and that’s a valid concern.
(Client usually appears surprised and relieved at this point.)
The veterinary professional: You aren’t the only person who has heard that. When I heard about the study, I researched it myself, because I was worried about my pets. What I found is that the British study that linked autism to vaccines, the one that scared all the parents, was retracted about six years ago because the study was proven false. The Centers for Disease Control and Prevention has published a resource center that goes into great detail about the safety of vaccines if you’d like more information.
Infectious disease control represents a major part of our effort as your pet’s health care providers. Vaccines are better studied than any other medicine we prescribe, and the manufacturers guarantee their safety and efficacy.
The vaccines we recommend are the vaccines we think your pet needs. I made sure my pet got these vaccines, and if Bella were my pet, I would be getting these vaccines for her to make sure she is as safe and healthy as she can be. Is that OK?
(Hopefully, at this point the client nods head and smiles. She might even say …)
Client: Thank you for explaining that. And not thinking I was crazy.
The veterinary professional: Of course. I know you want the best for your pet. You and I want the same thing. It’s my job to help you with these concerns.
“In 16 years of practice, using this approach, I never had anybody say no to the core vaccines after that discussion because however emotionally attached they were to their position beforehand, when they actually saw all the pros and cons of it, they realized it’s probably just better to get this thing done,” Dr. Wooten said.
Used with permission from dvm360.com