
January 01, 2021
Getting ahead of osteoarthritis in pets
In dogs, unlike humans, osteoarthritis actually tends to start at a young age. In cats, osteoarthritis is exceedingly common. Yet, the disease often goes undiagnosed and untreated in pets.
A diagnosis of osteoarthritis in a pet can be unwelcome to the veterinarian as well as the pet owner because the disease is painful and progressive, but experts say earlier diagnosis and treatment are pivotal to managing both the pain and the progression of the disease.
At the AVMA Virtual Convention 2020 in August, professors from two veterinary colleges gave talks about treating canine osteoarthritis effectively—including by using a new staging tool—and integrating new types of treatments for pets with osteoarthritis. At the American Association of Feline Practitioners’ virtual conference in October 2020, the owner of a feline-only practice discussed how to manage feline osteoarthritis cases.

Treating dogs
Dr. B. Duncan X. Lascelles, professor of surgery and pain management at North Carolina State University College of Veterinary Medicine, spoke at the AVMA Virtual Convention 2020 on “When and How, Treating Canine OA Effectively.”
In humans, Dr. Lascelles said, osteoarthritis is an older person’s disease. People erroneously superimpose that fact on dogs, but osteoarthritis in dogs mostly results from developmental problems. He said, “Osteoarthritis is a young dog’s disease.”
Then, when does osteoarthritis pain actually start in dogs? Dr. Lascelles said pain starts in younger dogs, but they adapt their posture to continue daily living activities. The pain has deleterious effects such as musculoskeletal deterioration, central sensitization, and cognitive and affective decline. All of these result in increased resistance to treatment.

“We don’t want to make a diagnosis of OA in young dogs. We see OA as an incurable lifelong disease, and we don’t want to have what we think is a depressing conversation about this with owners of younger dogs,” Dr. Lascelles said. “Actually, I think that we should have that conversation with owners but turn it around and make it more optimistic. ‘I’m glad we made this diagnosis because now we have the opportunity to improve your dog’s future.’”
Dr. Lascelles was part of the group that developed the new Canine OsteoArthritis Staging Tool. COAST is available from Elanco at jav.ma/coast or by calling 888-545-5973.
The first step of COAST is to grade the dog through owner assessments, via a clinical metrology instrument and owner observation of the dog’s discomfort, and through a veterinarian’s evaluation of the dog’s static posture and motion. The second step of COAST is for the veterinarian to grade the problematic joint on the basis of severity of signs of pain during manipulation, passive range of movement, and radiographic appearance.
The last step of COAST is to assign a numerical stage ranging from 0-4. Stage 0 is clinically normal with no risk factors for osteoarthritis, stage 1 is clinically normal with risk factors for osteoarthritis, stage 2 is mild osteoarthritis, stage 3 is moderate osteoarthritis, and stage 4 is severe osteoarthritis.
Dr. Lascelles said the four pillars of treatment for osteoarthritis in dogs are an effective analgesic such as a nonsteroidal anti-inflammatory drug, weight optimization, diet optimization, and exercise. The treatments are interdependent. An effective analgesic decreases pain, which allows for an increase in exercise. Exercise contributes to weight management, and exercise and weight management together decrease pain. Finally, a decrease in pain allows for a decrease in the analgesic requirement.
Dr. Lascelles shared his basic six-month approach to all patients with osteoarthritis pain. For three months, he prescribes an analgesic, a gradual increase in exercise, omega-3 fatty acids in a supplement or special diet, and reduction of food by a third with the addition of green beans, broccoli, or carrots. For the next three months, he reduces the dose or frequency of the analgesic, maintains exercise and diet, and further optimizes or maintains weight.
Treatments old and new
Dr. Bryan T. Torres, an assistant professor of small animal orthopedic surgery at the University of Missouri College of Veterinary Medicine, spoke at the AVMA Virtual Convention 2020 on “Osteoarthritis Management: Integrating New & Emerging Therapies Into Your Current Treatment Plans,” during the New Therapeutic Approaches to Chronic Care Symposium.
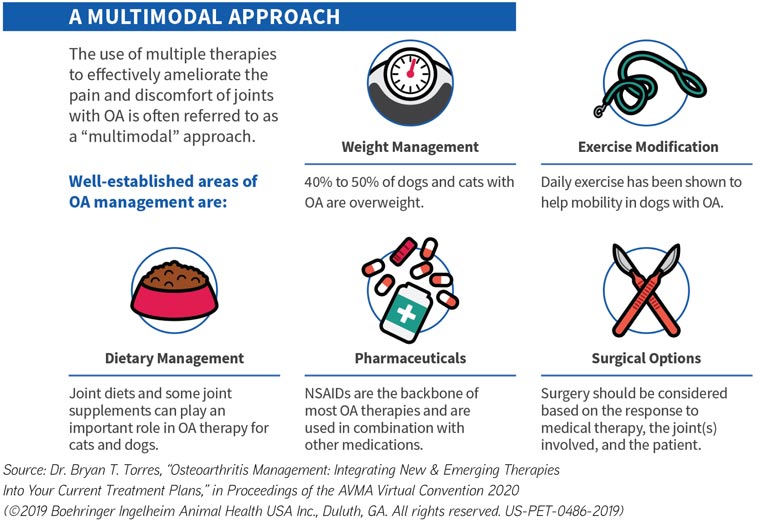
Dr. Torres considers the fundamentals of osteoarthritis management to be weight management, exercise modification, dietary management, drugs, and surgery. He said surgical options are always available but should be most strongly considered when medical management alone has reached its limits.

One of the emerging areas of osteoarthritis management is monoclonal antibody–based agents that are being developed—but that are not yet commercially available—to target cellular components that affect osteoarthritis pain and inflammation, such as cytokines, chemokines, and neurotrophins. Studies have found that monoclonal antibodies targeting nerve growth factor, a neurotrophic factor, reduce pain in humans, dogs, and cats with osteoarthritis.
Intra-articular treatments historically have included corticosteroids and hyaluronic acid, but other intra-articular treatments currently available include platelet-rich plasma and stem cells. There is some evidence that the latter two can be effective in animals with osteoarthritis, but most studies are of small populations with variability in treatments, joints affected, and disease severity.
Another currently available intra-articular treatment is radiosynovectomy, or the use of radioactive agents to reduce inflammation and chondromalacia in patients with osteoarthritis. Unfortunately, Dr. Torres said, there are no peer-reviewed studies available yet.
Cannabinoids also have potential for treating osteoarthritis in animals. Receptors for cannabinoids are present throughout joints, and the human literature has data supporting use of cannabinoids for pain. The evidence to support the efficacy of cannibidiol is currently limited but growing in veterinary medicine.
“Integrating new therapies can be challenging,” Dr. Torres said. “Just dealing with patients with this common condition can seem challenging. It can seem overwhelming because we have so many options out there, but that’s good, as long as we have a grasp of what to do and how to do it.
“And I think the keys to remember are that in most cases, we’re going to start with these foundational therapies, right? Weight management, exercise modification, dietary management, drug therapy, surgical therapy. These are going to work in most of the animals, and this is the way to start.”
Treating cats
Dr. Elizabeth Colleran, owner of Chico Hospital for Cats in Chico, California, spoke at the 2020 AAFP virtual conference about “Pouncing on Pain: Managing Feline Osteoarthritis Cases.”
Dr. Colleran described cats as solitary hunters that have limited social communication and are deliberately inscrutable. They manifest pain through reductions in play, grooming, socializing, and appetite and increases in hiding and sleeping. Dr. Colleran cited a study led by Dr. Lascelles that found 91% of cats between 6 months old and 20 years old have radiographic evidence of osteoarthritis in at least one joint.

To evaluate pain in cats with osteoarthritis, Dr. Colleran uses the Feline Musculoskeletal Pain Index out of North Carolina State University. She said the FMPI is an evaluation of common behaviors and activities that take place in the household and that don’t really take place in the examination room. Cat owners also can use a smartphone to record cats at home in slow motion to allow a veterinarian to evaluate gait, play, and jumping.
When cat owners are resistant to the idea of osteoarthritis pain in their cat, Dr. Colleran often will put the cat on an anti-inflammatory medication such as robenacoxib or meloxicam or an analgesic such as buprenorphine and ask the owners to report back in a few days.
Recently, Dr. Colleran could tell that a cat had osteoarthritis just by touching his back, but she couldn’t convince the owner. So she put the cat on robenacoxib for three days, and the owner called back to say he hadn’t seen what was happening. She said, “He was so aghast at the fact that he had missed really significant osteoarthritis pain and was convinced not by my explanation in the exam room but by the experience he had of the change in behavior at home.”
Dr. Colleran said the components of a treatment plan for osteoarthritis in cats can include weight loss, pharmaceuticals, environmental enrichment or modification, and a special diet or omega-3 supplements.
“Usually, when we have some acute pain, we’ll start with opioids, add in some NSAIDs, and then start thinking about ways in which we can change the experience that the cat is having and improve quality of life,” Dr. Colleran said. “But in all of these, you need to prioritize the ones that are working for this cat and this client at this time.”